In the Apr 2013 issue of Int J Crit Illn Inj Science, the authors from Iran attempt to identify the sensitivity, specificity, positive predictive value and accuracy of the right subcostal diaphragm view in the immediately paralyzed and intubated patient to confirm endotracheal intubation (versus esophageal intubation). This study comes from prior studies done suggesting that by visualizing diaphragm movement with ventilation or BVM, you can ascertain that the ET tube was placed in the trachea and not the esophagus. This adds to the growing number of studies that also discusses visualization of the lung sliding sign after intubation to confirm endotracheal intubation, and the ease at which you can identify the tube in the trachea and the esophagus upon trans-jugular notch view and identification of the ring down artifact through the trachea or a tube shadow beyond the esophagus, respectively.
To view a prior post on airway US and ETT placement confirmation, go here. For a fun airway guided talk by Ultrasound Podcast on it all, go here, and here.
So, after you intubate – look over the jugular notch for the ring down artifact through the trachea with the absence of esophageal shadow, then look for lung sliding on both sides of the chest with BVM or ventilation (this can also assess for pneumothorax prior to intubation), then look at the diaphragm for movement with ventilation post intubation. None will show you exactly where the end of the ET tube is, but you’ll know that youre not in the esophagus with good confidence – especially if your capnography isnt accurate due to post- cardiac arrest and your Xray machine/tech is busy or in the bathroom.
The abstract is below:
Aims:
To assess the sensitivity and specificity of right subcostal ultrasound view to confirm correct endotracheal tube intubation (ETT).
Materials and Methods:
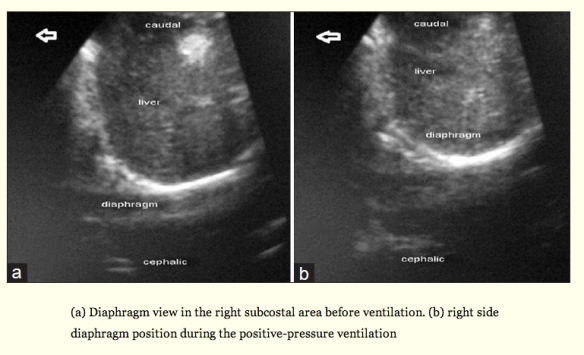
In this prospective study, apneic or paralyzed patients who had an indication of intubation were selected. Intubation and ventilation with bag were performed by the skilled third-year emergency medicine residents. The residents, following a brief training course of ultrasonography, interpreted the diaphragm motion, and identified either esophageal or tracheal intubation. The confirmation of ETT placement was done by the sonographer. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated for tracheal versus esophageal intubation.
Results:
A total of 57 patients aged 59 ± 5 who underwent ETT insertion were studied. Thirty-four of them were male (60%). Ultrasound correctly identified 11 out of 12 esophageal intubations for a sensitivity of 92% (95% CI = 62-100), but misidentified one esophageal intubation as tracheal. Sonographers correctly identified 43 out of 45 (96%) tracheal intubations for a specificity of 96% (95% CI = 85-99), but misdiagnosed two tracheal intubations as esophageal.
Conclusions:
This study suggests that diaphragm motion in right subcostal ultrasound view is an effective adjunct to diagnose ETT place in patients undergoing intubation in emergency department.
Likely the best description from the article is below:”…Studies have shown that ultrasound can diagnose paralyzed diaphragm.[16,17] Therefore, it seems practical to detect diaphragm motion during the positive-pressure ventilation by using ultrasound imaging of it. Hsieh, et al. studied the use of diaphragm motion for confirmation of ETT correct placement on 59 children in prenatal intensive care unit (PICU) setting. They diagnosed all intubations correctly with ultrasound imaging with sensitivity and specificity of 100%; however, they had only two esophageal intubations.[25] Kerrey, et al.[26] used diaphragm motion view of ultrasound in confirmation of correct ETT placement in 66 children in PICU. They evaluated the diagnosis of right main bronchus intubation. In their study, the sensitivity and specificity were 88% and 64%, respectively. Although sensitivity and specificity of the ultrasound in our study were high, we cannot strongly state that the ultrasound is a sensitive and specific method, because the confidence interval for sensitivity and specificity were rather wide. Studies have identified the intubation of the right main bronchus using diaphragm motion or observation of the lung sliding sign by placing the probe in the left side of the chest; however, left side of the chest is not as good as the right side for seeing the diaphragm motion.[22,26] If the patient is paralyzed or apneic, it would be suitable to evaluate the diaphragm motion in the right side of the chest to diagnose the esophageal intubation.”